Vitamin C megadosage: Difference between revisions
m Dated {{Clarify}}. (Build p608) |
→Cancer: Ichim et al 2011 |
||
| Line 25: | Line 25: | ||
=== Cancer === |
=== Cancer === |
||
In 1976 [[Linus Pauling]] and [[Ewan Cameron]] published a trial of 100 patients which suggested that treatment with intravenous vitamin C significantly increased lifespans.<ref name=PNAS1976/> Three large, placebo-controlled trials of only oral (not intravenous asorbic acid, as with Paulings' study) vitamin C in 1979, 1983 and 1985<ref name = Creagan/><ref name = Moertel/><ref name = Tschetter/> did not find a positive effect of vitamin C in cancer patients and a re-analysis of Pauling and Cameron's initial data found that the comparison groups were not adequately controlled or randomized, with the vitamin C group being less sick than controls when entering the study.<ref name = DeWys/><ref name = Quackwatch/> More recent Phase I clinical trial studies, which were limited in scope to a "dose-finding phase," have confirmed that while vitamin C is not necessarily [[Toxicity|toxic]] to cancer patients,<ref name=pilotcancer>{{cite journal |author=Riordan HD, Casciari JJ, González MJ, ''et al.'' |title=A pilot clinical study of continuous intravenous ascorbate in terminal cancer patients |journal=P R Health Sci J |volume=24 |issue=4 |pages=269–276 |year=2005 |month=December |pmid=16570523 |doi= |url=}}</ref> it is not useful as a treatment for cancer in humans when doses do not exceed 1.5 grams ascorbic acid/kg body weight.<ref name=PhaseIcancer/> ''[[In vitro]]'' tests on cell lines indicate that [[dehydroascorbic acid]] (DHA), an oxidized form of ascorbic acid may interfere with the effectiveness of [[chemotherapy]].<ref>{{cite journal |author=Heaney ML, Gardner JR, Karasavvas N, ''et al.'' |title=Vitamin C antagonizes the cytotoxic effects of antineoplastic drugs |journal=Cancer Res. |volume=68 |issue=19 |pages=8031–8038 |year=2008 |month=October |pmid=18829561 |doi=10.1158/0008-5472.CAN-08-1490 |url=}}</ref> A systematic review of the use of vitamin C and other antioxidants as part of a chemotherapeutic regimen found no significant difference between groups.<ref>{{cite pmid | 17367938 }}</ref> A 2010 review of 33 years of research on vitamin C to treat cancer stated "we have to conclude that we still do not know whether Vitamin C has any clinically significant antitumor activity. Nor do we know which histological types of cancers, if any, are susceptible to this agent. Finally, we don't know what the recommended dose of Vitamin C is, if there is indeed such a dose, that can produce an anti-tumor response."<ref>{{cite pmid | 20799507 }}</ref> No treatment protocols currently exist that involve vitamin C as a main or secondary chemotherapeutic agent, though there have been calls to re-evaluate the potential for vitamin C as a treatment for cancer patients.<ref>{{cite pmid | 19414313 }}</ref> |
In 1976 [[Linus Pauling]] and [[Ewan Cameron]] published a trial of 100 patients which suggested that treatment with intravenous vitamin C significantly increased lifespans.<ref name=PNAS1976/> Three large, placebo-controlled trials of only oral (not intravenous asorbic acid, as with Paulings' study) vitamin C in 1979, 1983 and 1985<ref name = Creagan/><ref name = Moertel/><ref name = Tschetter/> did not find a positive effect of vitamin C in cancer patients and a re-analysis of Pauling and Cameron's initial data found that the comparison groups were not adequately controlled or randomized, with the vitamin C group being less sick than controls when entering the study.<ref name = DeWys/><ref name = Quackwatch/> More recent Phase I clinical trial studies, which were limited in scope to a "dose-finding phase," have confirmed that while vitamin C is not necessarily [[Toxicity|toxic]] to cancer patients,<ref name=pilotcancer>{{cite journal |author=Riordan HD, Casciari JJ, González MJ, ''et al.'' |title=A pilot clinical study of continuous intravenous ascorbate in terminal cancer patients |journal=P R Health Sci J |volume=24 |issue=4 |pages=269–276 |year=2005 |month=December |pmid=16570523 |doi= |url=}}</ref> it is not useful as a treatment for cancer in humans when doses do not exceed 1.5 grams ascorbic acid/kg body weight.<ref name=PhaseIcancer/> ''[[In vitro]]'' tests on cell lines indicate that [[dehydroascorbic acid]] (DHA), an oxidized form of ascorbic acid may interfere with the effectiveness of [[chemotherapy]].<ref>{{cite journal |author=Heaney ML, Gardner JR, Karasavvas N, ''et al.'' |title=Vitamin C antagonizes the cytotoxic effects of antineoplastic drugs |journal=Cancer Res. |volume=68 |issue=19 |pages=8031–8038 |year=2008 |month=October |pmid=18829561 |doi=10.1158/0008-5472.CAN-08-1490 |url=}}</ref> A systematic review of the use of vitamin C and other antioxidants as part of a chemotherapeutic regimen found no significant difference between groups.<ref>{{cite pmid | 17367938 }}</ref> A 2010 review of 33 years of research on vitamin C to treat cancer stated "we have to conclude that we still do not know whether Vitamin C has any clinically significant antitumor activity. Nor do we know which histological types of cancers, if any, are susceptible to this agent. Finally, we don't know what the recommended dose of Vitamin C is, if there is indeed such a dose, that can produce an anti-tumor response."<ref>{{cite pmid | 20799507 }}</ref> No treatment protocols currently exist that involve vitamin C as a main or secondary chemotherapeutic agent, though there have been calls to re-evaluate the potential for vitamin C as a treatment for cancer patients.<ref>{{cite pmid | 19414313 }}</ref> |
||
In March 2011 a peer reviewed article in the ''Jounal of Translational Medicine'' concluded that there was a proven role for high doses of Ascorbic acid in the amelioration of cancer-associated inflammation. <ref>[http://www.translational-medicine.com/content/pdf/1479-5876-9-25.pdf Intravenous ascorbic acid to prevent and treat cancer-associated sepsis?] Ichim et al. Journal of Translational Medicine 2011, 9:25. Accessed April 2011</ref> |
|||
===Treatment of phencyclidine psychosis=== |
===Treatment of phencyclidine psychosis=== |
||
Revision as of 23:34, 5 April 2011
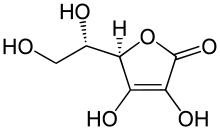

Vitamin C megadosage is the consumption (or injection) of vitamin C (ascorbate) in doses well beyond the current Dietary Reference Intake.[clarification needed] Such doses are similar to the consumption of ascorbate in other primates which, like humans, cannot synthesize their own vitamin C.[1] Nearly all other animals synthesize vitamin C internally. As such, their cellular vitamin C concentrations are considerably higher than those achieved with the Reference Daily Intake set for humans.[2]
Vitamin C is a recognized antioxidant, which has led to its endorsement by some researchers as a complementary therapy for improving quality of life.[3] Vitamin C has been promoted in alternative medicine as a treatment for the common cold, cancer, polio and various other illnesses. The evidence for these claims is mixed, although vitamin C is generally regarded as a beneficial antioxidant. There is a strong advocacy movement for such doses of vitamin C, despite a prolonged lack of conclusive medical evidence or large scale, formal trials in the 10 to 200+ grams per day range.
Background
Vitamin C is needed in the diet to prevent scurvy; however, since the 1930s, when it first became available in pure form, some physicians have experimented with vitamin C as a treatment for diseases other than scurvy.[4] Orthomolecular-based megadose recommendations for vitamin C are based mainly on theoretical speculation and observational studies. The speculation arises from the fact that most animals synthesize vitamin C and achieve much higher cellular concentrations than humans. Irwin Stone coined the term hypoascorbia to describe what he thought was a genetic defect in humans leading to a lower level of vitamin C than other primates. Observational studies began with work by McCormick and Klenner, who used intravenous (IV) vitamin C to treat a wide range of illnesses. The highest dose treatments - published clinical results of specific orthomolecular therapy regimens pioneered by Drs. Klenner (repeated IV treatments, 400–700+ (mg/kg)/day[5][6]) and Cathcart (oral use until the onset of diarrhea,[7] up to ~150 grams ascorbate per day for flu) - have remained experimentally unaddressed by conventional medical authorities for decades.
A comprehensive systematic review of vitamin C and the cold found a minor effect (8% for adults, 14% for children) of reducing the cold's duration, but vitamin C failed to reduce the cold's occurrence in general cases, excluding extreme environments; a substantial reduction of the cold's occurrence (50%) was noticed, however, in "marathon runners, skiers, and soldiers exposed to significant cold and/or physical stress." [8] The minimum dose rate in the studies examined (0.2g) was much lower than the dose advocated by megavitamin proponents. Its effect on cancer has been controversial, beginning with a heavily criticized[9] 1976 study which alleged to find significantly increased survival among cancer patients treated with intravenous and oral vitamin C.[10] Three subsequent studies using oral ascorbate failed to replicate these findings;[11][12][13] the original series was criticized for failing to randomize and control the treatment versus placebo groups,[14] and vitamin C's use as a cancer treatment was dismissed by mainstream medicine.[9][15] Recently, research has found that high dose i.v. vitamin C, which was found to kill in vitro cancer cells through the generation of hydrogen peroxide,[16] and tests of intravenous vitamin C on cancer patients, are not toxic, though they were also found to be ineffective at killing cancer cells or shrinking tumours.[17]
Conditions
Common cold
The results of three meta-analyses show vitamin C in doses ranging from 200 mg to 2 grams per day reduces the duration, but not the incidence, of the common cold by 8% for adults and 14% for children. Incidence appears to be reduced by 50% in stressed adults, such as soldiers or athletes, in extreme cold environments. The clinical significance of these effects is uncertain, but the biological effect appears genuine.[8][18]
A 2010 Cochrane Review concluded:[19]
The failure of vitamin C supplementation to reduce the incidence of colds in the general population indicates that routine prophylaxis is not justified. Vitamin C could be useful for people exposed to brief periods of severe physical exercise. While the prophylaxis trials have consistently shown that vitamin C reduces the duration and alleviates the symptoms of colds, this was not replicated in the few therapeutic trials that have been carried out. Further therapeutic RCTs are warranted.
Heart disease
Clinical trials investigating the use of vitamin C in the prevention of coronary disease or strokes have produced equivocal results, with positive, negative and neutral outcomes that make the studies difficult to interpret.[20]
Cancer
In 1976 Linus Pauling and Ewan Cameron published a trial of 100 patients which suggested that treatment with intravenous vitamin C significantly increased lifespans.[10] Three large, placebo-controlled trials of only oral (not intravenous asorbic acid, as with Paulings' study) vitamin C in 1979, 1983 and 1985[11][12][13] did not find a positive effect of vitamin C in cancer patients and a re-analysis of Pauling and Cameron's initial data found that the comparison groups were not adequately controlled or randomized, with the vitamin C group being less sick than controls when entering the study.[14][15] More recent Phase I clinical trial studies, which were limited in scope to a "dose-finding phase," have confirmed that while vitamin C is not necessarily toxic to cancer patients,[21] it is not useful as a treatment for cancer in humans when doses do not exceed 1.5 grams ascorbic acid/kg body weight.[17] In vitro tests on cell lines indicate that dehydroascorbic acid (DHA), an oxidized form of ascorbic acid may interfere with the effectiveness of chemotherapy.[22] A systematic review of the use of vitamin C and other antioxidants as part of a chemotherapeutic regimen found no significant difference between groups.[23] A 2010 review of 33 years of research on vitamin C to treat cancer stated "we have to conclude that we still do not know whether Vitamin C has any clinically significant antitumor activity. Nor do we know which histological types of cancers, if any, are susceptible to this agent. Finally, we don't know what the recommended dose of Vitamin C is, if there is indeed such a dose, that can produce an anti-tumor response."[24] No treatment protocols currently exist that involve vitamin C as a main or secondary chemotherapeutic agent, though there have been calls to re-evaluate the potential for vitamin C as a treatment for cancer patients.[25]
In March 2011 a peer reviewed article in the Jounal of Translational Medicine concluded that there was a proven role for high doses of Ascorbic acid in the amelioration of cancer-associated inflammation. [26]
Treatment of phencyclidine psychosis
Large dosages of vitamin C can be used to augment an antipsychotic in the treatment of acute phencyclidine (PCP) psychosis. Usually, 1000–2000 mg. of vitamin C are given intravenously over the course of 5–10 minutes. It is given in combination with a DA-2 antagonist such as haloperidol or risperidone. The antagonist is given intramuscularly and not combined with vitamin C. The vitamin acts synergistically with phencyclidine or its metabolites.[27]
Gout
In 2008, researchers established that higher vitamin C intake (diet or supplements) reduces serum uric acid levels and is associated with lower incidence of gout. The relative risk of gout was 45% lower for intakes of over 1500mg/d. [28]
Lifespan
A study published in 1992 suggested that men who took 800 mg of vitamin C daily lived approximately six years longer than men who took only 60 mg of vitamin C daily,[29] though there were substantial differences between the groups aside from vitamin intake. For example, because correlation does not imply causation, it is difficult to determine whether the extended lifespan was due to increased vitamin intake or whether other factors (e.g. greater concern regarding health and disease or greater disposable income to spend on vitamin supplements) may have caused both the extended lifespan and an increased vitamin intake.[30]
Possible adverse effects
While being harmless in most typical quantities, as with all substances to which the human body is exposed, vitamin C can still cause harm under certain conditions. In the medical community, these are known as contraindications.
- As vitamin C enhances iron absorption for iron deficiency, iron overload may become an issue to people with rare iron-overload conditions, such as Beta (β) thalassemias and hemochromatosis.[citation needed]
- A genetic condition that results in inadequate levels of the enzyme glucose-6-phosphate dehydrogenase (G6PD) can cause sufferers to develop hemolytic anemia after ingesting specific oxidizing substances (favism), such as very large dosages of vitamin C. Common, inexpensive tests exist to determine G6PD deficiency.[citation needed]
- There is a longstanding belief among the mainstream medical community that vitamin C causes kidney stones, which seems based little on science.[31] Although some individual recent studies have found a relationship,[32] there is no clear relationship between excess ascorbic acid intake and kidney stone formation.[33]
Side effects
Blood levels of vitamin C remain steady at approximately 200 mg per day. Although vitamin C can be well tolerated at doses well above the RDA recommendations, adverse effects can occur at doses above 3 grams per day though overload is unlikely. Possible adverse effects of megadoses include diarrhea, increased oxalate excretion and kidney stones, increased uric acid excretion, systemic conditioning ("rebound scurvy"), preoxidant effects, iron overload, reduced absorption of vitamin B12 and copper, increased oxygen demand and acid erosion of the teeth.[34] In addition, one case has been noted of a woman who had received a kidney transplant followed by high-dose vitamin C and died soon afterwards as a result of calcium oxalate deposits that destroyed her new kidney. Her doctors concluded that high-dose vitamin C therapy should be avoided in patients with renal failure.[35]
Chance of overdose
As discussed previously, vitamin C generally exhibits low toxicity. The LD50 (the dose that will kill 50% of a population) is generally accepted to be 11900 milligrams [11.9 grams] per kilogram in rat populations.[36] This is equivalent to a 70 kilogram human ingesting 850 grams of vitamin C.
Conflicts with prescription drugs
Pharmaceuticals designed to reduce stomach acid, such as the proton pump inhibitors (PPIs), are among the most widely-sold drugs in the world. One PPI, omeprazole (Prilosec), has been found to lower the bioavailability of vitamin C by 12% after 28 days of treatment, independent of dietary intake. The probable mechanism of vitamin C reduction, intragastric pH elevated into alkalinity, would apply to all other PPI drugs, though not necessarily to doses of PPIs low enough to keep the stomach slightly acidic.[37]. In another study, 40 mg/day of omeprazole lowered the fasting gastric vitamin C levels from 3.8 to 0.7 microg/mL. [38]
Aspirin may also inhibit the absorption of vitamin C.[39][40][41]
Potential harmful effects
- Some test-tube experiments have interpreted that vitamin C may have possible adverse effects on decomposition of lipid peroxides[42] in nonviable in vivo quantities and conditions,[43] and inhibit caspase-8 dependent apoptosis.[44] In April 1998 the journal Nature reported pro-oxidant effects of excessive doses of vitamin C / ascorbic acid.[45] The effects were noted in test tube experiments and on only two of the 20 markers of free radical damage to DNA. They have not been supported by further evidence from living organisms.[43]
- In June 2004, Duke University researchers reported an increased susceptibility to osteoarthritis in guinea pigs fed a diet high in vitamin C. However, a 2003 study at Umeå University in Sweden, found that "the plasma levels of vitamin C, retinol and uric acid were inversely correlated to variables related to rheumatoid arthritis disease activity."
- A speculated increased risk of kidney stones may be a side effect of taking vitamin C in larger than normal amounts (more than 1 gram). The potential mechanism of action is through the metabolism of vitamin C to dehydroascorbic acid, which is then metabolized to oxalic acid,[46] a known constituent of kidney stones. However, this oxalate issue is still controversial, with evidence being presented for[47] and against[48] the possibility of this side effect.
- "Rebound scurvy" is a theoretical, never observed, condition that could occur when daily intake of vitamin C is rapidly reduced from a very large amount to a relatively low amount. Advocates suggest this is an exaggeration of the rebound effect which occurs because ascorbate-dependent enzyme reactions continue for 24–48 hours after intake is lowered, and use up vitamin C which is not being replenished.
- Some writers[49] have identified a risk of poor copper absorption from high doses of vitamin C. Ceruloplasmin levels seem specifically lowered by high vitamin C intake. In one study, 600 milligrams of vitamin C daily led to lower ceruloplasmin levels similar to those caused by copper deficiency.[50] In another, ceruloplasmin levels were significantly reduced.[51]
- Long term use of high-dose vitamin C supplements may be associated with increased incidence of age-related cataract in older women.[52]
Genetic deficiency and broad spectrum hypotheses

Since its discovery vitamin C has been considered almost a universal panacea[citation needed] by some, although this led to suspicions of it being overhyped by others.[53]
Humans and higher primates, as well as guinea pigs and small number of other animal species, carry a mutated and ineffective form of the enzyme L-gulonolactone oxidase, the fourth and last step in the ascorbate-producing machinery. This mutation likely occurred 40 to 25 million years ago (in the anthropoids lineage). The three surviving enzymes continue to produce the precursors to vitamin C, but the process is incomplete and the body then disassembles them.
In the 1960s, the Nobel-Prize-winning chemist Linus Pauling, after contact with Irwin Stone, began actively promoting vitamin C as a means to greatly improve human health and resistance to disease. His book How to Live Longer and Feel Better was a bestseller and advocated taking more than 10,000 milligrams per day orally, thus approaching the amounts released by the liver directly into the circulation in other mammals: an adult goat, a typical example of a vitamin-C-producing animal, will manufacture more than 13,000 mg of vitamin C per day in normal health and as much as 100,000 mg daily when faced with life-threatening disease, trauma, or stress.[54]
Matthias Rath is a controversial German physician who worked with Pauling and published in the Proceedings of the National Academy of Sciences.[55][56] He is an active proponent and publicist for high dose vitamin C. Pauling's and Rath's extended theory states that deaths from scurvy in humans during the ice age, when vitamin C was scarce, selected for individuals who could repair arteries with a layer of cholesterol provided by lipoprotein(a), a lipoprotein found in vitamin C-deficient species (higher primates and guinea pigs).[57]
Genetic rationales for high doses
Four gene products are necessary to manufacture vitamin C from glucose. The loss of activity of the gene for the last step, Pseudogene ΨGULO (GLO), the terminal enzyme responsible for manufacture of vitamin C, has occurred separately in the history of several species. The loss of this enzyme activity is responsible for the inability of guinea pigs to synthesize vitamin C enzymatically, but this event happened independently of the loss in the haplorrhini suborder of primates, including humans. The remains of this non-functional gene with many mutations are, however, still present in the genome of the guinea pigs and in primates, including humans.[58][59] GLO activity has also been lost in all major families of bats, regardless of diet.[60] In addition, the function of GLO appears to have been lost several times, and possibly reacquired, in several lines of passerine birds, where ability to make vitamin C varies from species to species.[61]
Loss of GLO activity in the primate order supposedly occurred about 63 million years ago, at about the time it split into the suborders haplorrhini (which lost the enzyme activity) and the more primitive strepsirrhini (which retained it). The haplorrhini ("simple nosed") primates, which cannot make vitamin C enzymatically, include the tarsiers and the simians (apes, monkeys and humans). The suborder strepsirrhini (bent or wet-nosed prosimians), which are still able to make vitamin C enzymatically, include lorises, galagos, pottos, and to some extent, lemurs.[62]
Stone[63] and Pauling[64] calculated, based on the diet of our primate cousins[65] (similar to what our common ancestors are likely to have consumed when the gene mutated), that the optimum daily requirement of vitamin C is around 2,300 milligrams for a human requiring 2,500 kcal a day.
Pauling criticized the established US Recommended Daily Allowance, pointing out that it is based on the known quantities that will prevent acute scurvy but is not necessarily the dosage for optimal health.[66]
Regulation of vitamin C
Regulation
There are regulations in most countries which limit the claims on the treatment of disease that can be placed on food, drug, and nutrient product labels. Regulations include:
- Claims of therapeutic effect with respect to the treatment of any medical condition or disease are prohibited by the Food and Drug Administration in the USA, and by the corresponding regulatory agencies in other countries, unless the substance has gone through a well established clinical trial with neutral oversight.
- In the United States, the following notice is mandatory on food, drug, and nutrient product labels which make health claims: These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure or prevent any disease.[67]
Advocacy arguments
Vitamin C advocates argue that there is a large body of scientific evidence that the vitamin has a wide range of health and therapeutic benefits but that this has been ignored. They claim the following factors affect the marketing and distribution of vitamin C, and the dissemination of information concerning the nutrient:[68]
- There is some evidence regarding the applications and efficacy of vitamin C, but recommended governmental agency doses and frequency of intake have remained relatively fixed. This has led some researchers to challenge the recommendations. In 2003, Steve Hickey and Hilary Roberts of the Manchester Metropolitan University published a fundamental criticism of the approach taken to fix the nutritional requirement of vitamin C. In 2004, they again argued that the RDA, which is based on blood plasma and white blood cell saturation data from the National Institutes of Health (NIH), was based on flawed data.[69] According to these authors, the doses required to achieve blood, tissue and body "saturation" are much larger than previously believed. They allege that the Institute of Medicine (IoM) and the NIH have failed to respond to an open letter from a number of scientists and medical researchers, notably Doctors Steve Hickey, Hilary Roberts, Ian Brighthope, Robert Cathcart, Abram Hoffer, Archie Kalokerinos, Tom Levy, Richard Passwater, Hugh Riordan, Andrew Saul and Patrick Holford, which called for revision of the RDI (Reference Daily Intake).
See also
- Ascorbic acid
- Micronutrient
- Macronutrient
- Megavitamin therapy
- Orthomolecular medicine
- Uric acid
- Vitamin
References
- ^ Pauling L (1970). "Evolution and the need for ascorbic acid". Proc. Natl. Acad. Sci. U.S.A. 67 (4): 1643–1648. doi:10.1073/pnas.67.4.1643. PMC 283405. PMID 5275366.
{{cite journal}}:|access-date=requires|url=(help) - ^ Stone, Irwin. Homo sapiens ascorbicus, a biochemically corrected robust human mutant. Med. Hypotheses 5: 711–722, 1979. Online Mendelian Inheritance in Man.
- ^ Yeom CH, Jung GC, Song KJ (2007). "Changes of terminal cancer patients' health-related quality of life after high dose vitamin C administration". J. Korean Med. Sci. 22 (1): 7–11. doi:10.3346/jkms.2007.22.1.7. PMC 2693571. PMID 17297243.
{{cite journal}}:|access-date=requires|url=(help)CS1 maint: multiple names: authors list (link)". - ^ "Vitamin C (Ascorbic Acid)". University of Maryland Medical Center. 2002. Retrieved 2007-02-19.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Frederick Robert Klenner. "Significance of High Daily Intake of Ascorbic Acid in Preventive Medicine". AscorbateWeb. Retrieved 2007-02-19.
- ^ Frederick R. Klenner. "Observations On the Dose and Administration of Ascorbic Acid When Employed Beyond the Range of A Vitamin In Human Pathology". AscorbateWeb. Retrieved 2007-02-19.
- ^ Robert F. Cathcart III (1996). "Preparation of Sodium Ascorbate for IV and IM Use". orthomed.com. Retrieved 2007-02-21.
- ^ a b Douglas RM, Hemilä H (2005). "Vitamin C for Preventing and Treating the Common Cold". PLoS Medicine. 2 (6): e168. doi:10.1371/journal.pmed.0020168. PMC 1160577. PMID 15971944.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Trevor Pinch; Collins, Harry M. (2005). "Alternative Medicine: The Cases of Vitamin C and Cancer". Dr. Golem: how to think about medicine. Chicago: University of Chicago Press. pp. 89–111. ISBN 0-226-11366-3.
{{cite book}}:|access-date=requires|url=(help); External link in|chapterurl=|chapterurl=ignored (|chapter-url=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ a b Cameron E, Pauling L (1976). "Supplemental ascorbate in the supportive treatment of cancer: Prolongation of survival times in terminal human cancer". PNAS. 73 (10): 3685–3689. doi:10.1073/pnas.73.10.3685. PMC 431183. PMID 1068480.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ a b Creagan ET, Moertel CG, O'Fallon JR; et al. (1979). "Failure of high-dose vitamin C (ascorbic acid) therapy to benefit patients with advanced cancer. A controlled trial". NEJM. 301 (13): 687–690. doi:10.1056/NEJM197909273011303. PMID 384241.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Moertel CG, Fleming TR, Creagan ET, Rubin J, O'Connell MJ, Ames MM (1985). "High-dose vitamin C versus placebo in the treatment of patients with advanced cancer who have had no prior chemotherapy. A randomized double-blind comparison". NEJM. 312 (3): 137–141. doi:10.1056/NEJM198501173120301. PMID 3880867.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Tschetter, L (1983). "A community-based study of vitamin C (ascorbic acid) in patients with advanced cancer". Proceedings of the American Society of Clinical Oncology. 2: 92.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ a b DeWys, WD (1982). "How to evaluate a new treatment for cancer". Your Patient and Cancer. 2 (5): 31–36.
- ^ a b Barrett, S (2008-10-23). "High Doses of Vitamin C Are Not Effective as a Cancer Treatment". Quackwatch. Retrieved 2010-05-06.
- ^ Chen Q, Espey MG, Krishna MC; et al. (2005). "Pharmacologic ascorbic acid concentrations selectively kill cancer cells: action as a pro-drug to deliver hydrogen peroxide to tissues". Proc. Natl. Acad. Sci. U.S.A. 102 (38): 13604–13609. doi:10.1073/pnas.0506390102. PMC 1224653. PMID 16157892.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ a b Hoffer LJ, Levine M, Assouline S; et al. (2008). "Phase I clinical trial of i.v. ascorbic acid in advanced malignancy". Ann. Oncol. 19 (11): 1969. doi:10.1093/annonc/mdn377. PMID 18544557.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Gorton, HC, (1999 Oct;22). "The effectiveness of vitamin C in preventing and relieving the symptoms of virus-induced respiratory infections". Journal of Manipulative and Physiological Therapeutics. 8. PubMed: 530–533.
{{cite journal}}: Check date values in:|date=(help); Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: extra punctuation (link) CS1 maint: multiple names: authors list (link) - ^ Hemilä, H (2000). "Vitamin C for preventing and treating the common cold". Cochrane Database of Systematic Reviews. 3 (2): CD000980. doi:10.1002/14651858.CD000980. ISSN 1464-780X. PMID 10796569.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20400494, please use {{cite journal}} with
|pmid= 20400494instead. - ^ Riordan HD, Casciari JJ, González MJ; et al. (2005). "A pilot clinical study of continuous intravenous ascorbate in terminal cancer patients". P R Health Sci J. 24 (4): 269–276. PMID 16570523.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Heaney ML, Gardner JR, Karasavvas N; et al. (2008). "Vitamin C antagonizes the cytotoxic effects of antineoplastic drugs". Cancer Res. 68 (19): 8031–8038. doi:10.1158/0008-5472.CAN-08-1490. PMID 18829561.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 17367938 , please use {{cite journal}} with
|pmid= 17367938instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 20799507 , please use {{cite journal}} with
|pmid= 20799507instead. - ^ Attention: This template ({{cite pmid}}) is deprecated. To cite the publication identified by PMID 19414313 , please use {{cite journal}} with
|pmid= 19414313instead. - ^ Intravenous ascorbic acid to prevent and treat cancer-associated sepsis? Ichim et al. Journal of Translational Medicine 2011, 9:25. Accessed April 2011
- ^ Giannini AJ, Loiselle RH, DiMarzio LR, Giannini MC (1987). "Augmentation of haloperidol by ascorbic acid in phencyclidine intoxication". The American journal of psychiatry. 144 (9): 1207–1209. PMID 3631319.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Choi, MD, DrPH, Hyon K. (March 9, 2009). "Vitamin C Intake and the Risk of Gout in Men". Archives of Internal Medicine. 169 (5): 502–507. doi:10.1001/archinternmed.2008.606. PMC 2767211. PMID 19273781.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: multiple names: authors list (link) - ^ Enstrom JE, Kanim LE, Klein MA (1992). "Vitamin C intake and mortality among a sample of the United States population". Epidemiology. 3 (3): 194–202. doi:10.1097/00001648-199205000-00003. PMID 1591317.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Kim I, Williamson DF, Byers T, Koplan JP (1994). "Vitamin Supplement Use and Mortality". Am J Public Health. 84 (6): 1035–1037. doi:10.2105/AJPH.84.6.1035. PMC 1614952. PMID 8460732.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Goodwin JS, Tangum MR (1998). "Battling quackery: attitudes about micronutrient supplements in American academic medicine". Arch. Intern. Med. 158 (20): 2187–2191. doi:10.1001/archinte.158.20.2187. PMID 9818798.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Massey LK, Liebman M, Kynast-Gales SA (2005). "Ascorbate increases human oxaluria and kidney stone risk" (PDF). J. Nutr. 135 (7): 1673–1677. PMID 15987848.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Naidu KA (2003). "Vitamin C in human health and disease is still a mystery? An overview" (PDF). J. Nutr. 2 (7): 7. doi:10.1186/1475-2891-2-7. PMC 201008. PMID 14498993.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Dietary reference intakes for vitamin C, vitamin E, selenium, and carotenoids: a report of the Panel on Dietary Antioxidants and Related Compounds, Subcommittees on Upper Reference Levels of Nutrients and of Interpretation and Use of Dietary Reference Intakes, and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Washington, D.C: National Academy Press. 2000. pp. 156–161. ISBN 0-309-06949-1.
- ^ Nankivell, BJ (2008). "Renal failure from vitamin C after transplantation" (PDF). NEJM. 358 (4): e4. doi:10.1056/NEJMicm070984. PMID 18216350.
{{cite journal}}: Unknown parameter|coauthors=ignored (|author=suggested) (help) - ^ "Safety (MSDS) data for ascorbic acid". Oxford University. October 9, 2005. Retrieved 2007-02-21.
- ^ E. B. Henry, A. Carswell, A. Wirz, V. Fyffe & K. E. L. Mccoll (2005). "Proton pump inhibitors reduce the bioavailability of dietary vitamin C". Alimentary Pharmacology & Therapeutics. Retrieved 2007-02-21.
The gastric-juice concentration of vitamin C is reduced in subjects with elevated intragastric pH. This is probably because the vitamin is unstable at non-acidic pH and undergoes irreversible denaturation. After 28 days of 40 mg/day of omeprazole, the mean plasma vitamin C level had fallen by 12.3% (P = 0.04).
{{cite web}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ C. Mowat, A. Carswell, A. Wirz, K.E. McColl (1999). "Omeprazole and dietary nitrate independently affect levels of vitamin C and nitrite in gastric juice". Alimentary Pharmacology & Therapeutics. Retrieved 2011-02-14.
{{cite web}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Loh HS, Watters K & Wilson CW (1 November 1973). "The Effects of Aspirin on the Metabolic Availability of Ascorbic Acid in Human Beings". J Clin Pharmacol. 13 (11): 480–486. PMID 4490672.
- ^ Basu TK (1982). "Vitamin C-aspirin interactions". Int J Vitam Nutr Res Suppl. 23: 83–90. PMID 6811490.
- ^ Ioannides C, Stone AN, Breacker PJ & Basu TK (1982). "Impairment of absorption of ascorbic acid following ingestion of aspirin in guinea pigs". Biochem Pharmacol. 31 (24): 4035–4038. doi:10.1016/0006-2952(82)90652-9. PMID 6818974.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ [1] Vitamin C produces gene-damaging compounds Accessed July 2007
- ^ a b Balz Frei, Ph.D. (November, 2001). "Vitamin C Doesn't Cause Cancer!". Oregon State University. Retrieved 2007-02-21.
{{cite web}}: Check date values in:|date=(help) - ^ Perez-Cruz I, Cárcamo JM, Golde DW (2007). "Caspase-8 dependent TRAIL-induced apoptosis in cancer cell lines is inhibited by vitamin C and catalase". Apoptosis. 12 (1): 225–234. doi:10.1007/s10495-006-0475-0. PMID 17031493.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ian D. Podmore, Helen R. Griffiths, Karl E. Herbert, Nalini Mistry, Pratibha Mistry and Joseph Lunec (9 April 1998). "Vitamin C exhibits pro-oxidant properties". Nature. 392 (6676): 559. doi:10.1038/33308. PMID 9560150.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hokama S, Toma C, Jahana M; et al. (2000). "Ascorbate conversion to oxalate in alkaline milieu and Proteus mirabilis culture". Mol Urol. 4 (4): 321–328. PMID 11156698.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Massey LK, Liebman M, Kynast-Gales SA (2005). "Ascorbate increases human oxaluria and kidney stone risk". J Nutr. 123 (7): 1673. PMID 15987848.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Stephen Lawson (November 1999). "What About Vitamin C and Kidney Stones?". The Linus Pauling Institute. Retrieved 2007-02-21.
- ^ acu-cell
- ^ Jacob RA, Skala JH, Omaye ST, Turnlund JR. (1987). "Effect of varying ascorbic acid intakes on copper absorption and ceruloplasmin levels of young men". J Nutr. 117 (12): 2109–2115. PMID 3694287.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Finley EB, Cerklewski FL (1983). "Influence of ascorbic acid supplementation on copper status in young adult men". Am J Clin Nutr. 37 (4): 553–556. PMID 6837490.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Rautiainen S, Lindblad BE, Morgenstern R, Wolk A (2010). "Vitamin C supplements and the risk of age-related cataract: a population-based prospective cohort study in women". The American Journal of Clinical Nutrition. 91 (2): 487–493. doi:10.3945/ajcn.2009.28528. PMID 19923367.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Harri Hemilä (2006). "Do vitamins C and E affect respiratory infections?" (PDF). University of Helsinki. Retrieved 2007-02-21.
{{cite web}}: Unknown parameter|month=ignored (help) - ^ Stone, Irwin (July 16, 1978). "Eight Decades of Scurvy. The Case History of a Misleading Dietary Hypothesis". Retrieved 2007-04-06.
Biochemical research in the 1950s showed that the lesion in scurvy is the absence of the enzyme, L-Gulonolactone oxidase (GLO) in the human liver (Burns, 1959). This enzyme is the last enzyme in a series of four, which converts blood sugar (glucose) into ascorbate in the mammalian liver. This liver metabolite, ascorbate, is produced in an unstressed goat, for instance, at the rate of about 13,000 mg per day per 150 pounds body weight (Chatterjee, 1973). A mammalian feedback mechanism increases this daily ascorbate production many fold under stress (Subramanian et al., 1973)
{{cite web}}: Cite has empty unknown parameter:|coauthors=(help) - ^ Rath M, Pauling L (1990). "Immunological evidence for the accumulation of lipoprotein(a) in the atherosclerotic lesion of the hypoascorbemic guinea pig". Proc Natl Acad Sci USA. 87 (23): 9388–9390. doi:10.1073/pnas.87.23.9388. PMC 55170. PMID 2147514.
- ^ Rath M, Pauling L (1990). "Hypothesis: lipoprotein(a) is a surrogate for ascorbate". Proc Natl Acad Sci USA. 87 (16): 6204–6207. doi:10.1073/pnas.87.16.6204. PMC 54501. PMID 2143582.
- ^ Rath M, Pauling L (1992). "A unified theory of human cardiovascular disease leading the way to the abolition of this disease as a cause for human mortality" (PDF). Journal of Orthomolecular Medicine. 7 (1): 5–15.
- ^ Nishikimi M, Kawai T, Yagi K (25 October 1992). "Guinea pigs possess a highly mutated gene for L-gulono-gamma-lactone oxidase, the key enzyme for L-ascorbic acid biosynthesis missing in this species". J Biol Chem. 267 (30): 21967–21972. PMID 1400507.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ohta Y, Nishikimi M (1999). "Random nucleotide substitutions in primate nonfunctional gene for L-gulono-gamma-lactone oxidase, the missing enzyme in L-ascorbic acid biosynthesis". Biochim Biophys Acta. 1472 (1–2): 408–411. PMID 10572964.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ A trace of GLO was detected in only 1 of 34 bat species tested, across the range of 6 families of bats tested: See Jenness R, Birney E, Ayaz K (1980). "Variation of L-gulonolactone oxidase activity in placental mammals". Comparative Biochemistry and Physiology. 67B: 195–204.
{{cite journal}}: CS1 maint: multiple names: authors list (link) Earlier reports of only fruit bats being deficient were based on smaller samples. - ^ Carlos Martinez del Rio (1997). "Can passerines synthesize vitamin C?". The Auk.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Pollock JI, Mullin RJ (1987). "Vitamin C biosynthesis in prosimians: evidence for the anthropoid affinity of Tarsius". Am J Phys Anthropol. 73 (1): 65–70. doi:10.1002/ajpa.1330730106. PMID 3113259.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Stone, Irwin (1972). The Healing Factor: Vitamin C Against Disease. Grosset and Dunlap. ISBN 0-448-11693-6. OCLC 3967737.
- ^ Pauling, Linus (1970). "Evolution and the need for ascorbic acid". Proc Natl Acad Sci USA. 67 (4): 1643–1648. doi:10.1073/pnas.67.4.1643. PMC 283405. PMID 5275366.
- ^ Milton K (2003). "Micronutrient intakes of wild primates: are humans different?" (PDF). Comp Biochem Physiol a Mol Integr Physiol. 136 (1): 47–59. doi:10.1016/S1095-6433(03)00084-9. PMID 14527629.
- ^ Pauling, Linus (1986). How to Live Longer and Feel Better. W. H. Freeman and Company. ISBN 0-380-70289-4. OCLC 154663991 15690499.
{{cite book}}: Check|oclc=value (help) - ^ "Dietary Supplement Health and Education Act of 1994".
- ^ Richards E (1988). "The Politics of Therapeutic Evaluation: The Vitamin C and Cancer Controversy". Social Studies of Science. 18 (4): 653–701. doi:10.1177/030631288018004004.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Hickey S, Roberts H (2005). "Misleading information on the properties of vitamin C". PLoS Med. 2 (9): e307, author reply e309. doi:10.1371/journal.pmed.0020307. PMC 1236801. PMID 16173838.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: unflagged free DOI (link)
External links
- The Vitamin C Foundation principal organisition promoting megadosage. Accessed July 2007
- Quackwatch article critical of megadosing Charles W. Marshall, Ph.D. Accessed July 2007
