Herd immunity

Herd immunity (also called herd effect, community immunity, population immunity, or mass immunity) is a form of indirect protection that applies only to contagious diseases. It occurs when a sufficient percentage of a population has become immune to an infection, whether through previous infections or vaccination,[1] thereby reducing the likelihood of infection for individuals who lack immunity.[2][3][4]
Once the herd immunity has been reached, disease gradually disappears from a population and may result in eradication or permanent reduction of infections to zero if achieved worldwide.[5][6] Herd immunity created via vaccination has contributed to the reduction of many diseases.[7]
Effects[edit]
Protection of those without immunity[edit]

Some individuals either cannot develop immunity after vaccination or for medical reasons cannot be vaccinated.[8][9][10] Newborn infants are too young to receive many vaccines, either for safety reasons or because passive immunity renders the vaccine ineffective.[11] Individuals who are immunodeficient due to HIV/AIDS, lymphoma, leukemia, bone marrow cancer, an impaired spleen, chemotherapy, or radiotherapy may have lost any immunity that they previously had and vaccines may not be of any use for them because of their immunodeficiency.[9][10][11][12]
A portion of those vaccinated may not develop long-term immunity.[2][13][14] Vaccine contraindications may prevent certain individuals from being vaccinated.[10] In addition to not being immune, individuals in one of these groups may be at a greater risk of developing complications from infection because of their medical status, but they may still be protected if a large enough percentage of the population is immune.[9][10][14][15]
High levels of immunity in one age group can create herd immunity for other age groups.[7] Vaccinating adults against pertussis reduces pertussis incidence in infants too young to be vaccinated, who are at the greatest risk of complications from the disease.[16][17] This is especially important for close family members, who account for most of the transmissions to young infants.[7][14] In the same manner, children receiving vaccines against pneumococcus reduces pneumococcal disease incidence among younger, unvaccinated siblings.[18] Vaccinating children against pneumococcus and rotavirus has had the effect of reducing pneumococcus- and rotavirus-attributable hospitalizations for older children and adults, who do not normally receive these vaccines.[18][19][20] Influenza (flu) is more severe in the elderly than in younger age groups, but influenza vaccines lack effectiveness in this demographic due to a waning of the immune system with age.[7][21] The prioritization of school-age children for seasonal flu immunization, which is more effective than vaccinating the elderly, however, has been shown to create a certain degree of protection for the elderly.[7][21]
For sexually transmitted infections (STIs), high levels of immunity in heterosexuals of one sex induces herd immunity for heterosexuals of both sexes.[22][23][24] Vaccines against STIs that are targeted at heterosexuals of one sex result in significant declines in STIs in heterosexuals of both sexes if vaccine uptake in the target sex is high.[23][24][25] Herd immunity from female vaccination does not, however, extend to males who have sex with males.[24] High-risk behaviors make eliminating STIs difficult because, even though most infections occur among individuals with moderate risk, the majority of transmissions occur because of individuals who engage in high-risk behaviors.[22] For this reason, in certain populations it may be necessary to immunize high-risk individuals regardless of sex.[22][24]
Evolutionary pressure and serotype replacement[edit]
Herd immunity itself acts as an evolutionary pressure on pathogens, influencing viral evolution by encouraging the production of novel strains, referred to as escape mutants, that are able to evade herd immunity and infect previously immune individuals.[26][27] The evolution of new strains is known as serotype replacement, or serotype shifting, as the prevalence of a specific serotype declines due to high levels of immunity, allowing other serotypes to replace it.[28][29]
At the molecular level, viruses escape from herd immunity through antigenic drift, which is when mutations accumulate in the portion of the viral genome that encodes for the virus's surface antigen, typically a protein of the virus capsid, producing a change in the viral epitope.[30][31] Alternatively, the reassortment of separate viral genome segments, or antigenic shift, which is more common when there are more strains in circulation, can also produce new serotypes.[26][32] When either of these occur, memory T cells no longer recognize the virus, so people are not immune to the dominant circulating strain.[31][32] For both influenza and norovirus, epidemics temporarily induce herd immunity until a new dominant strain emerges, causing successive waves of epidemics.[30][32] As this evolution poses a challenge to herd immunity, broadly neutralizing antibodies and "universal" vaccines that can provide protection beyond a specific serotype are in development.[27][33][34]
Initial vaccines against Streptococcus pneumoniae significantly reduced nasopharyngeal carriage of vaccine serotypes (VTs), including antibiotic-resistant types,[18][35] only to be entirely offset by increased carriage of non-vaccine serotypes (NVTs).[18][28][29] This did not result in a proportionate increase in disease incidence though, since NVTs were less invasive than VTs.[28] Since then, pneumococcal vaccines that provide protection from the emerging serotypes have been introduced and have successfully countered their emergence.[18] The possibility of future shifting remains, so further strategies to deal with this include expansion of VT coverage and the development of vaccines that use either killed whole-cells, which have more surface antigens, or proteins present in multiple serotypes.[18][36]
Eradication of diseases[edit]

If herd immunity has been established and maintained in a population for a sufficient time, the disease is inevitably eliminated – no more endemic transmissions occur.[5] If elimination is achieved worldwide and the number of cases is permanently reduced to zero, then a disease can be declared eradicated.[6] Eradication can thus be considered the final effect or end-result of public health initiatives to control the spread of contagious disease.[6][7] In cases in which herd immunity is compromised, on the contrary, disease outbreaks among the unvaccinated population are likely to occur.[37]
The benefits of eradication include ending all morbidity and mortality caused by the disease, financial savings for individuals, health care providers, and governments, and enabling resources used to control the disease to be used elsewhere.[6] To date, two diseases have been eradicated using herd immunity and vaccination: rinderpest and smallpox.[2][7][38] Eradication efforts that rely on herd immunity are currently underway for poliomyelitis, though civil unrest and distrust of modern medicine have made this difficult.[2][39] Mandatory vaccination may be beneficial to eradication efforts if not enough people choose to get vaccinated.[40][41][42][43]
Free riding[edit]
Herd immunity is vulnerable to the free rider problem.[44] Individuals who lack immunity, including those who choose not to vaccinate, free ride off the herd immunity created by those who are immune.[44] As the number of free riders in a population increases, outbreaks of preventable diseases become more common and more severe due to loss of herd immunity.[45][46][47][41][43] Individuals may choose to free ride or be hesitant to vaccinate for a variety of reasons, including the belief that vaccines are ineffective,[48] or that the risks associated with vaccines are greater than those associated with infection,[2][46][47][48] mistrust of vaccines or public health officials,[49] bandwagoning or groupthinking,[41][50] social norms or peer pressure,[48] and religious beliefs.[46] Certain individuals are more likely to choose not to receive vaccines if vaccination rates are high enough to convince a person that he or she may not need to be vaccinated, since a sufficient percentage of others are already immune.[2][43]
Mechanism[edit]
Individuals who are immune to a disease act as a barrier in the spread of disease, slowing or preventing the transmission of disease to others.[51] An individual's immunity can be acquired via a natural infection or through artificial means, such as vaccination.[51] When a critical proportion of the population becomes immune, called the herd immunity threshold (HIT) or herd immunity level (HIL), the disease may no longer persist in the population, ceasing to be endemic.[5][26]
The theoretical basis for herd immunity generally assumes that vaccines induce solid immunity, that populations mix at random, that the pathogen does not evolve to evade the immune response, and that there is no non-human vector for the disease.[2]
Theoretical basis[edit]
The critical value, or threshold, in a given population, is the point where the disease reaches an endemic steady state, which means that the infection level is neither growing nor declining exponentially. This threshold can be calculated from the effective reproduction number Re, which is obtained by taking the product of the basic reproduction number R0, the average number of new infections caused by each case in an entirely susceptible population that is homogeneous, or well-mixed, meaning each individual is equally likely to come into contact with any other susceptible individual in the population,[22][26][40] and S, the proportion of the population who are susceptible to infection, and setting this product to be equal to 1:[citation needed]
S can be rewritten as (1 − p), where p is the proportion of the population that is immune so that p + S equals one. Then, the equation can be rearranged to place p by itself as follows:[citation needed]
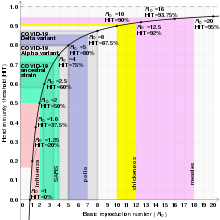
With p being by itself on the left side of the equation, it can be renamed as pc, representing the critical proportion of the population needed to be immune to stop the transmission of disease, which is the same as the "herd immunity threshold" HIT.[22] R0 functions as a measure of contagiousness, so low R0 values are associated with lower HITs, whereas higher R0s result in higher HITs.[26][40] For example, the HIT for a disease with an R0 of 2 is theoretically only 50%, whereas a disease with an R0 of 10 the theoretical HIT is 90%.[26]
When the effective reproduction number Re of a contagious disease is reduced to and sustained below 1 new individual per infection, the number of cases occurring in the population gradually decreases until the disease has been eliminated.[22][26][52] If a population is immune to a disease in excess of that disease's HIT, the number of cases reduces at a faster rate, outbreaks are even less likely to happen, and outbreaks that occur are smaller than they would be otherwise.[2][22] If the effective reproduction number increases to above 1, then the disease is neither in a steady state nor decreasing in incidence, but is actively spreading through the population and infecting a larger number of people than usual.[41][52]
An assumption in these calculations is that populations are homogeneous, or well-mixed, meaning that every individual is equally likely to come into contact with any other individual, when in reality populations are better described as social networks as individuals tend to cluster together, remaining in relatively close contact with a limited number of other individuals. In these networks, transmission only occurs between those who are geographically or physically close to one another.[2][40][41] The shape and size of a network is likely to alter a disease's HIT, making incidence either more or less common.[26][40] Mathematical models can use contact matrices to estimate the likelihood of encounters and thus transmission.[53]
In heterogeneous populations, R0 is considered to be a measure of the number of cases generated by a "typical" contagious person, which depends on how individuals within a network interact with each other.[2] Interactions within networks are more common than between networks, in which case the most highly connected networks transmit disease more easily, resulting in a higher R0 and a higher HIT than would be required in a less connected network.[2][41] In networks that either opt not to become immune or are not immunized sufficiently, diseases may persist despite not existing in better-immunized networks.[41]
| Disease | Transmission | R0 | HIT[a] |
|---|---|---|---|
| Measles | Aerosol | 12–18[54][55] | 92–94% |
| Chickenpox (varicella) | Aerosol | 10–12[56] | 90–92% |
| Mumps | Respiratory droplets | 10–12[57] | 90–92% |
| COVID-19 (see values for specific strains below) | Respiratory droplets and aerosol | 2.9-9.5[58] | 65–89% |
| Rubella | Respiratory droplets | 6–7[b] | 83–86% |
| Polio | Fecal–oral route | 5–7[b] | 80–86% |
| Pertussis | Respiratory droplets | 5.5[63] | 82% |
| Smallpox | Respiratory droplets | 3.5–6.0[64] | 71–83% |
| HIV/AIDS | Body fluids | 2–5[65] | 50–80% |
| SARS | Respiratory droplets | 2–4[66] | 50–75% |
| Diphtheria | Saliva | 2.6 (1.7–4.3)[67] | 62% (41–77%) |
| Common cold (e.g., rhinovirus) | Respiratory droplets | 2–3[68][medical citation needed] | 50–67% |
| Mpox | Physical contact, body fluids, respiratory droplets, sexual (MSM) | 2.1 (1.1–2.7)[69][70] | 53% (22–63%) |
| Ebola (2014 outbreak) | Body fluids | 1.8 (1.4–1.8)[71] | 44% (31–44%) |
| Influenza (seasonal strains) | Respiratory droplets | 1.3 (1.2–1.4)[72] | 23% (17–29%) |
| Andes hantavirus | Respiratory droplets and body fluids | 1.2 (0.8–1.6)[73] | 16% (0–36%)[c] |
| Nipah virus | Body fluids | 0.5[74] | 0%[c] |
| MERS | Respiratory droplets | 0.5 (0.3–0.8)[75] | 0%[c] |
Overshoot[edit]
The cumulative proportion of individuals who get infected during the course of a disease outbreak can exceed the HIT. This is because the HIT does not represent the point at which the disease stops spreading, but rather the point at which each infected person infects fewer than one additional person on average. When the HIT is reached, the number of additional infections does not immediately drop to zero. The excess of the cumulative proportion of infected individuals over the theoretical HIT is known as the overshoot.[76][77][78]
Boosts[edit]
Vaccination[edit]
The primary way to boost levels of immunity in a population is through vaccination.[2][79] Vaccination is originally based on the observation that milkmaids exposed to cowpox were immune to smallpox, so the practice of inoculating people with the cowpox virus began as a way to prevent smallpox.[39] Well-developed vaccines provide protection in a far safer way than natural infections, as vaccines generally do not cause the diseases they protect against and severe adverse effects are significantly less common than complications from natural infections.[80][81]
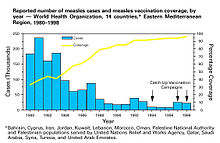
The immune system does not distinguish between natural infections and vaccines, forming an active response to both, so immunity induced via vaccination is similar to what would have occurred from contracting and recovering from the disease.[82] To achieve herd immunity through vaccination, vaccine manufacturers aim to produce vaccines with low failure rates, and policy makers aim to encourage their use.[79] After the successful introduction and widespread use of a vaccine, sharp declines in the incidence of diseases it protects against can be observed, which decreases the number of hospitalizations and deaths caused by such diseases.[83][84][85]
Assuming a vaccine is 100% effective, then the equation used for calculating the herd immunity threshold can be used for calculating the vaccination level needed to eliminate a disease, written as Vc.[2] Vaccines are usually imperfect however, so the effectiveness, E, of a vaccine must be accounted for:
From this equation, it can be observed that if E is less than (1 − 1/R0), then it is impossible to eliminate a disease, even if the entire population is vaccinated.[2] Similarly, waning vaccine-induced immunity, as occurs with acellular pertussis vaccines, requires higher levels of booster vaccination to sustain herd immunity.[2][16] If a disease has ceased to be endemic to a population, then natural infections no longer contribute to a reduction in the fraction of the population that is susceptible. Only vaccination contributes to this reduction.[22] The relation between vaccine coverage and effectiveness and disease incidence can be shown by subtracting the product of the effectiveness of a vaccine and the proportion of the population that is vaccinated, pv, from the herd immunity threshold equation as follows:
It can be observed from this equation that, all other things being equal ("ceteris paribus"), any increase in either vaccine coverage or vaccine effectiveness, including any increase in excess of a disease's HIT, further reduces the number of cases of a disease.[22] The rate of decline in cases depends on a disease's R0, with diseases with lower R0 values experiencing sharper declines.[22]
Vaccines usually have at least one contraindication for a specific population for medical reasons, but if both effectiveness and coverage are high enough then herd immunity can protect these individuals.[8][12][15] Vaccine effectiveness is often, but not always, adversely affected by passive immunity,[86][87] so additional doses are recommended for some vaccines while others are not administered until after an individual has lost his or her passive immunity.[11][15]
Passive immunity[edit]
Individual immunity can also be gained passively, when antibodies to a pathogen are transferred from one individual to another. This can occur naturally, whereby maternal antibodies, primarily immunoglobulin G antibodies, are transferred across the placenta and in colostrum to fetuses and newborns.[88][89] Passive immunity can also be gained artificially, when a susceptible person is injected with antibodies from the serum or plasma of an immune person.[82][90]
Protection generated from passive immunity is immediate, but wanes over the course of weeks to months, so any contribution to herd immunity is temporary.[5][82][91] For diseases that are especially severe among fetuses and newborns, such as influenza and tetanus, pregnant women may be immunized in order to transfer antibodies to the child.[8][92][93] In the same way, high-risk groups that are either more likely to experience infection, or are more likely to develop complications from infection, may receive antibody preparations to prevent these infections or to reduce the severity of symptoms.[90]
Cost–benefit analysis[edit]
Herd immunity is often accounted for when conducting cost–benefit analyses of vaccination programs. It is regarded as a positive externality of high levels of immunity, producing an additional benefit of disease reduction that would not occur had no herd immunity been generated in the population.[94][95] Therefore, herd immunity's inclusion in cost–benefit analyses results both in more favorable cost-effectiveness or cost–benefit ratios, and an increase in the number of disease cases averted by vaccination.[95] Study designs done to estimate herd immunity's benefit include recording disease incidence in households with a vaccinated member, randomizing a population in a single geographic area to be vaccinated or not, and observing the incidence of disease before and after beginning a vaccination program.[96] From these, it can be observed that disease incidence may decrease to a level beyond what can be predicted from direct protection alone, indicating that herd immunity contributed to the reduction.[96] When serotype replacement is accounted for, it reduces the predicted benefits of vaccination.[95]
History[edit]
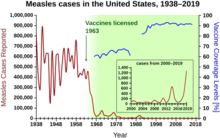
Herd immunity was recognized as a naturally occurring phenomenon in the 1930s when it was observed that after a significant number of children had become immune to measles, the number of new infections temporarily decreased.[97] Mass vaccination to induce herd immunity has since become common and proved successful in preventing the spread of many contagious diseases.[22] Opposition to vaccination has posed a challenge to herd immunity, allowing preventable diseases to persist in or return to populations with inadequate vaccination rates.[45][46][47]
The exact herd immunity threshold (HIT) varies depending on the basic reproduction number of the disease. An example of a disease with a high threshold was the measles, with a HIT exceeding 95%.[98]
The term "herd immunity" was first used in 1894 by American veterinary scientist and then Chief of the Bureau of Animal Industry of the US Department of Agriculture Daniel Elmer Salmon to describe the healthy vitality and resistance to disease of well-fed herds of hogs. In 1916 veterinary scientists inside the same Bureau of Animal Industry used the term to refer to the immunity arising following recovery in cattle infected with brucellosis, also known as "contagious abortion." By 1923 it was being used by British bacteriologists to describe experimental epidemics with mice, experiments undertaken as part of efforts to model human epidemic disease. By the end of the 1920s the concept was used extensively - particularly among British scientists - to describe the build up of immunity in populations to diseases such as diphtheria, scarlet fever, and influenza.[99] Herd immunity was recognized as a naturally occurring phenomenon in the 1930s when A. W. Hedrich published research on the epidemiology of measles in Baltimore, and took notice that after many children had become immune to measles, the number of new infections temporarily decreased, including among susceptible children.[100][97] In spite of this knowledge, efforts to control and eliminate measles were unsuccessful until mass vaccination using the measles vaccine began in the 1960s.[97] Mass vaccination, discussions of disease eradication, and cost–benefit analyses of vaccination subsequently prompted more widespread use of the term herd immunity.[2] In the 1970s, the theorem used to calculate a disease's herd immunity threshold was developed.[2] During the smallpox eradication campaign in the 1960s and 1970s, the practice of ring vaccination, to which herd immunity is integral, began as a way to immunize every person in a "ring" around an infected individual to prevent outbreaks from spreading.[101]
Since the adoption of mass and ring vaccination, complexities and challenges to herd immunity have arisen.[2][79] Modeling of the spread of contagious disease originally made a number of assumptions, namely that entire populations are susceptible and well-mixed, which is not the case in reality, so more precise equations have been developed.[2] In recent decades, it has been recognized that the dominant strain of a microorganism in circulation may change due to herd immunity, either because of herd immunity acting as an evolutionary pressure or because herd immunity against one strain allowed another already-existing strain to spread.[30][29] Emerging or ongoing fears and controversies about vaccination have reduced or eliminated herd immunity in certain communities, allowing preventable diseases to persist in or return to these communities.[45][46][47]
See also[edit]
Notes[edit]
References[edit]
- ^ "Herd immunity | immunology". Encyclopedia Britannica. Archived from the original on 1 April 2023. Retrieved 13 June 2021.
- ^ a b c d e f g h i j k l m n o p q r s Fine P, Eames K, Heymann DL (April 2011). ""Herd immunity": a rough guide". Clinical Infectious Diseases. 52 (7): 911–6. doi:10.1093/cid/cir007. PMID 21427399.
- ^ Gordis L (2013). Epidemiology. Elsevier Health Sciences. pp. 26–27. ISBN 978-1455742516. Archived from the original on 1 July 2023. Retrieved 29 March 2015.
- ^ "Cold-Causing Coronaviruses Don't Seem to Confer Lasting Immunity". The Scientist Magazine®. Archived from the original on 7 January 2021. Retrieved 26 January 2021.
- ^ a b c d Somerville M, Kumaran K, Anderson R (2012). Public Health and Epidemiology at a Glance. John Wiley & Sons. pp. 58–59. ISBN 978-1118308646. Archived from the original on 1 May 2021. Retrieved 29 March 2015.
- ^ a b c d Cliff, Smallman-Raynor M (2013). Oxford Textbook of Infectious Disease Control: A Geographical Analysis from Medieval Quarantine to Global Eradication. Oxford University Press. pp. 125–36. ISBN 978-0199596614. Archived from the original on 1 May 2021. Retrieved 29 March 2015.
- ^ a b c d e f g Kim TH, Johnstone J, Loeb M (September 2011). "Vaccine herd effect". Scandinavian Journal of Infectious Diseases. 43 (9): 683–9. doi:10.3109/00365548.2011.582247. PMC 3171704. PMID 21604922.
- ^ a b c Munoz FM (August 2013). "Maternal immunization: an update for pediatricians". Pediatric Annals. 42 (8): 153–8. doi:10.3928/00904481-20130723-09. PMID 23910028.
- ^ a b c "Herd Immunity". Oxford Vaccine Group, University of Oxford. Archived from the original on 2 August 2019. Retrieved 12 December 2017.
- ^ a b c d Cesaro S, Giacchino M, Fioredda F, Barone A, Battisti L, Bezzio S, et al. (2014). "Guidelines on vaccinations in paediatric haematology and oncology patients". BioMed Research International. 2014: 707691. doi:10.1155/2014/707691. PMC 4020520. PMID 24868544.
- ^ a b c National Center for Immunization Respiratory Diseases (January 2011). "General recommendations on immunization --- recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR. Recommendations and Reports. 60 (2): 1–64. PMID 21293327.
- ^ a b Wolfe RM (2012). "Update on adult immunizations". Journal of the American Board of Family Medicine. 25 (4): 496–510. doi:10.3122/jabfm.2012.04.100274. PMID 22773718.
- ^ Esposito S, Bosis S, Morlacchi L, Baggi E, Sabatini C, Principi N (October 2012). "Can infants be protected by means of maternal vaccination?". Clinical Microbiology and Infection. 18 (Suppl 5): 85–92. doi:10.1111/j.1469-0691.2012.03936.x. PMID 22862749.
- ^ a b c Rakel D, Rakel RE (2015). Textbook of Family Medicine. Elsevier Health Sciences. pp. 99, 187. ISBN 978-0323313087. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ a b c Tulchinsky TH, Varavikova EA (2014). The New Public Health: An Introduction for the 21st Century. Academic Press. pp. 163–82. ISBN 978-0124157675. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ a b McGirr A, Fisman DN (February 2015). "Duration of pertussis immunity after DTaP immunization: a meta-analysis" (PDF). Pediatrics. 135 (2): 331–43. doi:10.1542/peds.2014-1729. PMID 25560446. S2CID 8273985. Archived from the original (PDF) on 3 March 2019.
- ^ Zepp F, Heininger U, Mertsola J, Bernatowska E, Guiso N, Roord J, et al. (July 2011). "Rationale for pertussis booster vaccination throughout life in Europe". The Lancet. Infectious Diseases. 11 (7): 557–70. doi:10.1016/S1473-3099(11)70007-X. PMID 21600850.
- ^ a b c d e f Pittet LF, Posfay-Barbe KM (October 2012). "Pneumococcal vaccines for children: a global public health priority". Clinical Microbiology and Infection. 18 (Suppl 5): 25–36. doi:10.1111/j.1469-0691.2012.03938.x. PMID 22862432.
- ^ Nakagomi O, Iturriza-Gomara M, Nakagomi T, Cunliffe NA (November 2013). "Incorporation of a rotavirus vaccine into the national immunisation schedule in the United Kingdom: a review". Expert Opinion on Biological Therapy. 13 (11): 1613–21. doi:10.1517/14712598.2013.840285. PMID 24088009. S2CID 5405583.
- ^ Lopman BA, Payne DC, Tate JE, Patel MM, Cortese MM, Parashar UD (August 2012). "Post-licensure experience with rotavirus vaccination in high and middle income countries; 2006 to 2011". Current Opinion in Virology. 2 (4): 434–42. doi:10.1016/j.coviro.2012.05.002. PMID 22749491. Archived from the original on 16 October 2019. Retrieved 5 July 2019.
- ^ a b Kim TH (July 2014). "Seasonal influenza and vaccine herd effect". Clinical and Experimental Vaccine Research. 3 (2): 128–32. doi:10.7774/cevr.2014.3.2.128. PMC 4083064. PMID 25003085.
- ^ a b c d e f g h i j k Garnett GP (February 2005). "Role of herd immunity in determining the effect of vaccines against sexually transmitted disease". The Journal of Infectious Diseases. 191 (Suppl 1): S97-106. doi:10.1086/425271. PMID 15627236.
- ^ a b Lowy DR, Schiller JT (January 2012). "Reducing HPV-associated cancer globally". Cancer Prevention Research. 5 (1): 18–23. doi:10.1158/1940-6207.CAPR-11-0542. PMC 3285475. PMID 22219162.
- ^ a b c d Lenzi A, Mirone V, Gentile V, Bartoletti R, Ficarra V, Foresta C, et al. (February 2013). "Rome Consensus Conference - statement; human papilloma virus diseases in males". BMC Public Health. 13: 117. doi:10.1186/1471-2458-13-117. PMC 3642007. PMID 23391351.
- ^ Garland SM, Skinner SR, Brotherton JM (October 2011). "Adolescent and young adult HPV vaccination in Australia: achievements and challenges". Preventive Medicine. 53 (Suppl 1): S29-35. doi:10.1016/j.ypmed.2011.08.015. PMID 21962468.
- ^ a b c d e f g h Rodpothong, P; Auewarakul, P (2012). "Viral evolution and transmission effectiveness". World Journal of Virology. 1 (5): 131–34. doi:10.5501/wjv.v1.i5.131. PMC 3782273. PMID 24175217.
- ^ a b Corti, D; Lanzavecchia, A (2013). "Broadly neutralizing antiviral antibodies". Annual Review of Immunology. 31: 705–42. doi:10.1146/annurev-immunol-032712-095916. PMID 23330954.
- ^ a b c Weinberger, D. M.; Malley, R; Lipsitch, M (2011). "Serotype replacement in disease after pneumococcal vaccination". The Lancet. 378 (9807): 1962–73. doi:10.1016/S0140-6736(10)62225-8. PMC 3256741. PMID 21492929.
- ^ a b c McEllistrem, M. C.; Nahm, M. H. (2012). "Novel pneumococcal serotypes 6C and 6D: Anomaly or harbinger". Clinical Infectious Diseases. 55 (10): 1379–86. doi:10.1093/cid/cis691. PMC 3478140. PMID 22903767.
- ^ a b c Bull RA, White PA (May 2011). "Mechanisms of GII.4 norovirus evolution". Trends in Microbiology. 19 (5): 233–40. doi:10.1016/j.tim.2011.01.002. PMID 21310617.
- ^ a b Ramani S, Atmar RL, Estes MK (January 2014). "Epidemiology of human noroviruses and updates on vaccine development". Current Opinion in Gastroenterology. 30 (1): 25–33. doi:10.1097/MOG.0000000000000022. PMC 3955997. PMID 24232370.
- ^ a b c Pleschka S (2013). "Overview of Influenza Viruses". Swine Influenza. Current Topics in Microbiology and Immunology. Vol. 370. pp. 1–20. doi:10.1007/82_2012_272. ISBN 978-3642368707. PMID 23124938.
- ^ Han T, Marasco WA (January 2011). "Structural basis of influenza virus neutralization". Annals of the New York Academy of Sciences. 1217 (1): 178–90. Bibcode:2011NYASA1217..178H. doi:10.1111/j.1749-6632.2010.05829.x. PMC 3062959. PMID 21251008.
- ^ Reperant LA, Rimmelzwaan GF, Osterhaus AD (2014). "Advances in influenza vaccination". F1000Prime Reports. 6: 47. doi:10.12703/p6-47. PMC 4047948. PMID 24991424.
- ^ Dagan R (April 2009). "Impact of pneumococcal conjugate vaccine on infections caused by antibiotic-resistant Streptococcus pneumoniae". Clinical Microbiology and Infection. 15 (Suppl 3): 16–20. doi:10.1111/j.1469-0691.2009.02726.x. PMID 19366365.
- ^ Lynch JP, Zhanel GG (May 2010). "Streptococcus pneumoniae: epidemiology and risk factors, evolution of antimicrobial resistance, and impact of vaccines". Current Opinion in Pulmonary Medicine. 16 (3): 217–25. doi:10.1097/MCP.0b013e3283385653. PMID 20375783. S2CID 205784538.
- ^ Alhumaid, Saad; Al Mutair, Abbas; Al Alawi, Zainab; Rabaan, Ali A.; Tirupathi, Raghavendra; Alomari, Mohammed A.; Alshakhes, Aqeel S.; Alshawi, Abeer M.; Ahmed, Gasmelseed Y.; Almusabeh, Hassan M.; Alghareeb, Tariq T.; Alghuwainem, Abdulaziz A.; Alsulaiman, Zainab A.; Alabdulmuhsin, Mohammed A.; AlBuwaidi, Emad A.; Dukhi, Amjad K. Bu; Mufti, Hani N.; Al-Qahtani, Manaf; Dhama, Kuldeep; Al-Tawfiq, Jaffar A.; Al-Omari, Awad (December 2021). "Anaphylactic and nonanaphylactic reactions to SARS-CoV-2 vaccines: a systematic review and meta-analysis". Allergy, Asthma & Clinical Immunology. 17 (1): 109. doi:10.1186/s13223-021-00613-7. PMC 8520206. PMID 34656181.
- ^ Njeumi F, Taylor W, Diallo A, Miyagishima K, Pastoret PP, Vallat B, Traore M (December 2012). "The long journey: a brief review of the eradication of rinderpest". Revue Scientifique et Technique. 31 (3): 729–46. doi:10.20506/rst.31.3.2157. PMID 23520729.
- ^ a b Smith KA (May 2013). "Smallpox: can we still learn from the journey to eradication?". The Indian Journal of Medical Research. 137 (5): 895–9. PMC 3734679. PMID 23760373.
- ^ a b c d e Perisic A, Bauch CT (February 2009). "Social contact networks and disease eradicability under voluntary vaccination". PLOS Computational Biology. 5 (2): e1000280. Bibcode:2009PLSCB...5E0280P. doi:10.1371/journal.pcbi.1000280. PMC 2625434. PMID 19197342.
- ^ a b c d e f g Fu F, Rosenbloom DI, Wang L, Nowak MA (January 2011). "Imitation dynamics of vaccination behaviour on social networks" (PDF). Proceedings. Biological Sciences. 278 (1702): 42–9. doi:10.1098/rspb.2010.1107. PMC 2992723. PMID 20667876. Archived (PDF) from the original on 4 November 2018. Retrieved 4 November 2018.
- ^ Wicker S, Maltezou HC (August 2014). "Vaccine-preventable diseases in Europe: where do we stand?". Expert Review of Vaccines. 13 (8): 979–87. doi:10.1586/14760584.2014.933077. PMID 24958075. S2CID 23471069.
- ^ a b c Fukuda E, Tanimoto J (2014). Impact of Stubborn Individuals on a Spread of Infectious Disease under Voluntary Vaccination Policy. Springer. pp. 1–10. ISBN 978-3319133591. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ a b Barrett S (2014). "Global Public Goods and International Development". In J. Warren Evans, Robin Davies (eds.). Too Global To Fail: The World Bank at the Intersection of National and Global Public Policy in 2025. World Bank Publications. pp. 13–18. ISBN 978-1464803109.
- ^ a b c Quadri-Sheriff M, Hendrix KS, Downs SM, Sturm LA, Zimet GD, Finnell SM (September 2012). "The role of herd immunity in parents' decision to vaccinate children: a systematic review". Pediatrics. 130 (3): 522–30. doi:10.1542/peds.2012-0140. PMID 22926181.
- ^ a b c d e Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J (August 2013). "Vaccine hesitancy: an overview". Human Vaccines & Immunotherapeutics. 9 (8): 1763–73. doi:10.4161/hv.24657. PMC 3906279. PMID 23584253.
- ^ a b c d Ropeik D (August 2013). "How society should respond to the risk of vaccine rejection". Human Vaccines & Immunotherapeutics. 9 (8): 1815–8. doi:10.4161/hv.25250. PMC 3906287. PMID 23807359.
- ^ a b c Gowda C, Dempsey AF (August 2013). "The rise (and fall?) of parental vaccine hesitancy". Human Vaccines & Immunotherapeutics. 9 (8): 1755–62. doi:10.4161/hv.25085. PMC 3906278. PMID 23744504.
- ^ Ozawa S, Stack ML (August 2013). "Public trust and vaccine acceptance--international perspectives". Human Vaccines & Immunotherapeutics. 9 (8): 1774–8. doi:10.4161/hv.24961. PMC 3906280. PMID 23733039.
- ^ Parker AM, Vardavas R, Marcum CS, Gidengil CA (July 2013). "Conscious consideration of herd immunity in influenza vaccination decisions". American Journal of Preventive Medicine. 45 (1): 118–121. doi:10.1016/j.amepre.2013.02.016. PMC 3694502. PMID 23790997.
- ^ a b Merrill RM (2013). Introduction to Epidemiology. Jones & Bartlett Publishers. pp. 68–71. ISBN 978-1449645175. Archived from the original on 12 April 2021. Retrieved 29 March 2015.
- ^ a b Dabbaghian V, Mago VK (2013). Theories and Simulations of Complex Social Systems. Springer. pp. 134–35. ISBN 978-3642391491. Archived from the original on 1 May 2021. Retrieved 29 March 2015.
- ^ von Csefalvay, Chris (2023), "Host factors", Computational Modeling of Infectious Disease, Elsevier, pp. 93–119, doi:10.1016/b978-0-32-395389-4.00012-8, ISBN 978-0-323-95389-4
- ^ Guerra FM, Bolotin S, Lim G, Heffernan J, Deeks SL, Li Y, Crowcroft NS (December 2017). "The basic reproduction number (R0) of measles: a systematic review". The Lancet. Infectious Diseases. 17 (12): e420–e428. doi:10.1016/S1473-3099(17)30307-9. PMID 28757186.
- ^ Delamater PL, Street EJ, Leslie TF, Yang YT, Jacobsen KH (January 2019). "Complexity of the Basic Reproduction Number (R0)". Emerging Infectious Diseases. 25 (1): 1–4. doi:10.3201/eid2501.171901. PMC 6302597. PMID 30560777.
- ^ Ireland's Health Services. Health Care Worker Information (PDF). Retrieved 27 March 2020.
- ^ Australian government Department of Health Mumps Laboratory Case Definition (LCD)
- ^ Liu, Y (9 March 2022). "The effective reproductive number of the Omicron variant of SARS-CoV-2 is several times relative to Delta". Journal of Travel Medicine. 29 (3). Table 1. doi:10.1093/jtm/taac037. ISSN 1708-8305. PMC 8992231. PMID 35262737.
- ^ Centers for Disease Control and Prevention; World Health Organization (2001). "History and epidemiology of global smallpox eradication". Smallpox: disease, prevention, and intervention (training course) (Presentation). Atlanta: Centers for Disease Control and Prevention (published 25 August 2014). cdc:27929. Archived (PDF) from the original on 17 March 2017. Retrieved 17 June 2021.
- ^ Fine, Paul E. M. (1993). "Herd Immunity: History, Theory, Practice". Epidemiologic Reviews. 15 (2): 265–302. doi:10.1093/oxfordjournals.epirev.a036121. PMID 8174658.
- ^ Luman, ET; Barker, LE; Simpson, DM; Rodewald, LE; Szilagyi, PG; Zhao, Z (May 2001). "National, state, and urban-area vaccination-coverage levels among children aged 19–35 months, United States, 1999". American Journal of Preventive Medicine. 20 (4): 88–153. doi:10.1016/s0749-3797(01)00274-4. PMID 12174806.
- ^ Jiles, RB; Fuchs, C; Klevens, RM (22 September 2000). "Vaccination coverage among children enrolled in Head Start programs or day care facilities or entering school". Morbidity and Mortality Weekly Report. 49 (9): 27–38. PMID 11016876.
- ^ Kretzschmar M, Teunis PF, Pebody RG (June 2010). "Incidence and reproduction numbers of pertussis: estimates from serological and social contact data in five European countries". PLOS Medicine. 7 (6): e1000291. doi:10.1371/journal.pmed.1000291. PMC 2889930. PMID 20585374.
- ^ Gani R, Leach S (December 2001). "Transmission potential of smallpox in contemporary populations". Nature. 414 (6865): 748–51. Bibcode:2001Natur.414..748G. doi:10.1038/414748a. PMID 11742399. S2CID 52799168. Retrieved 18 March 2020.
- ^ "Playing the Numbers Game: R0". National Emerging Special Pathogen Training and Education Center. 30 January 2020. Archived from the original on 12 May 2020. Retrieved 27 December 2020.
[...] while infections that require sexual contact like HIV have a lower R0 (2-5).
- ^ Consensus document on the epidemiology of severe acute respiratory syndrome (SARS). Department of Communicable Disease Surveillance and Response (Technical report). World Health Organization. p. 26. hdl:10665/70863. WHO/CDS/CSR/GAR/2003.11.
A number of researchers have estimated the basic reproduction number by fitting models to the initial growth of epidemics in a number of countries. Their observations indicate that the SARS-CoV is less transmissible than initially thought with estimates of Ro in the range of 2-4.
- ^ Truelove SA, Keegan LT, Moss WJ, Chaisson LH, Macher E, Azman AS, Lessler J (June 2020). "Clinical and Epidemiological Aspects of Diphtheria: A Systematic Review and Pooled Analysis". Clinical Infectious Diseases. 71 (1): 89–97. doi:10.1093/cid/ciz808. PMC 7312233. PMID 31425581.
- ^ Freeman C (6 November 2014). "Magic formula that will determine whether Ebola is beaten". The Telegraph. Telegraph.Co.Uk. Archived from the original on 12 January 2022. Retrieved 30 March 2020.
- ^ Grant R, Nguyen LL, Breban R (1 September 2020). "Modelling human-to-human transmission of monkeypox" (PDF). Bulletin of the World Health Organization. 98 (9): 638–640. doi:10.2471/BLT.19.242347. ISSN 0042-9686. PMC 7463189. PMID 33012864. Archived from the original (PDF) on 11 December 2020.
- ^ Al-Raeei M (February 2023). "The study of human monkeypox disease in 2022 using the epidemic models: herd immunity and the basic reproduction number case". Annals of Medicine & Surgery. 85 (2): 316–321. doi:10.1097/MS9.0000000000000229. ISSN 2049-0801. PMC 9949786. PMID 36845803.
- ^ Wong ZS, Bui CM, Chughtai AA, Macintyre CR (April 2017). "A systematic review of early modelling studies of Ebola virus disease in West Africa". Epidemiology and Infection. 145 (6): 1069–1094. doi:10.1017/S0950268817000164. PMC 9507849. PMID 28166851.
The median of the R0 mean estimate for the ongoing epidemic (overall) is 1.78 (interquartile range: 1.44, 1.80)
- ^ Chowell G, Miller MA, Viboud C (June 2008). "Seasonal influenza in the United States, France, and Australia: transmission and prospects for control". Epidemiology and Infection. 136 (6). Cambridge University Press: 852–64. doi:10.1017/S0950268807009144. PMC 2680121. PMID 17634159.
The reproduction number across influenza seasons and countries lied in the range 0.9–2.0 with an overall mean of 1.3, and 95% confidence interval (CI) 1.2–1.4.
- ^ Martínez, Valeria P.; Di Paola, Nicholas; Alonso, Daniel O.; Pérez-Sautu, Unai; Bellomo, Carla M.; Iglesias, Ayelén A.; et al. (3 December 2020). "'Super-Spreaders' and Person-to-Person Transmission of Andes Virus in Argentina". New England Journal of Medicine. 383 (23): 2230–2241. doi:10.1056/NEJMoa2009040. PMID 33264545. S2CID 227259435.
- ^ Luby SP (October 2013). "The pandemic potential of Nipah virus". Antiviral Research. 100 (1): 38–43. doi:10.1016/j.antiviral.2013.07.011. PMID 23911335.
- ^ Kucharski AJ, Althaus CL (June 2015). "The role of superspreading in Middle East respiratory syndrome coronavirus (MERS-CoV) transmission". Euro Surveillance. 20 (25): 14–8. doi:10.2807/1560-7917.ES2015.20.25.21167. PMID 26132768.
- ^ Handel A, Longini IM, Antia R (March 2007). "What is the best control strategy for multiple infectious disease outbreaks?". Proceedings. Biological Sciences. 274 (1611): 833–7. doi:10.1098/rspb.2006.0015. PMC 2093965. PMID 17251095.
In general, the number of infecteds grows until the number of susceptibles has fallen to Sth. At this point, the average number of secondary infections created by an infected person drops below 1 and therefore the number of infecteds starts to decrease. However, right at this inflection point, the maximum number of infecteds is present. These infecteds will create on average less than 1, but still more than zero further infections, leading to additional depletion of susceptibles and therefore causing an overshoot.
- ^ Fung IC, Antia R, Handel A (11 June 2012). "How to minimize the attack rate during multiple influenza outbreaks in a heterogeneous population". PLOS ONE. 7 (6): e36573. Bibcode:2012PLoSO...736573F. doi:10.1371/journal.pone.0036573. PMC 3372524. PMID 22701558.
- ^ Bergstrom CT, Dean N (1 May 2020). "Opinion: What the Proponents of 'Natural' Herd Immunity Don't Say". The New York Times. Archived from the original on 3 June 2020. Retrieved 30 May 2020.
- ^ a b c Rashid H, Khandaker G, Booy R (June 2012). "Vaccination and herd immunity: what more do we know?". Current Opinion in Infectious Diseases. 25 (3): 243–9. doi:10.1097/QCO.0b013e328352f727. PMID 22561998. S2CID 19197608.
- ^ Maglione MA, Das L, Raaen L, Smith A, Chari R, Newberry S, et al. (August 2014). "Safety of vaccines used for routine immunization of U.S. children: a systematic review". Pediatrics. 134 (2): 325–37. doi:10.1542/peds.2014-1079. PMID 25086160. Archived from the original on 30 January 2020. Retrieved 5 July 2019.
- ^ Di Pietrantonj, Carlo; Rivetti, Alessandro; Marchione, Pasquale; Debalini, Maria Grazia; Demicheli, Vittorio (22 November 2021). "Vaccines for measles, mumps, rubella, and varicella in children". The Cochrane Database of Systematic Reviews. 2021 (11): CD004407. doi:10.1002/14651858.CD004407.pub5. ISSN 1469-493X. PMC 8607336. PMID 34806766.
- ^ a b c Pommerville JC (2014). Fundamentals of Microbiology: Body Systems Edition. Jones & Bartlett Publishers. pp. 559–63. ISBN 978-1284057102. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ Papaloukas O, Giannouli G, Papaevangelou V (March 2014). "Successes and challenges in varicella vaccine". Therapeutic Advances in Vaccines. 2 (2): 39–55. doi:10.1177/2051013613515621. PMC 3991154. PMID 24757524.
- ^ Shann F (February 2013). "Nonspecific effects of vaccines and the reduction of mortality in children". Clinical Therapeutics. 35 (2): 109–14. doi:10.1016/j.clinthera.2013.01.007. PMID 23375475.
- ^ Visser A, Hoosen A (September 2012). "Haemophilus influenzae type b conjugate vaccines - a South African perspective". Vaccine. 30 (Suppl 3): C52-7. doi:10.1016/j.vaccine.2012.06.022. hdl:2263/20792. PMID 22939022.
- ^ Leuridan E, Sabbe M, Van Damme P (September 2012). "Measles outbreak in Europe: susceptibility of infants too young to be immunized". Vaccine. 30 (41): 5905–13. doi:10.1016/j.vaccine.2012.07.035. PMID 22841972.
- ^ Hodgins DC, Shewen PE (February 2012). "Vaccination of neonates: problem and issues". Vaccine. 30 (9): 1541–59. doi:10.1016/j.vaccine.2011.12.047. PMID 22189699.
- ^ Chucri TM, Monteiro JM, Lima AR, Salvadori ML, Kfoury JR, Miglino MA (December 2010). "A review of immune transfer by the placenta". Journal of Reproductive Immunology. 87 (1–2): 14–20. doi:10.1016/j.jri.2010.08.062. PMID 20956021.
- ^ Palmeira P, Quinello C, Silveira-Lessa AL, Zago CA, Carneiro-Sampaio M (2012). "IgG placental transfer in healthy and pathological pregnancies". Clinical & Developmental Immunology. 2012: 985646. doi:10.1155/2012/985646. PMC 3251916. PMID 22235228.
- ^ a b Parija SC (2014). Textbook of Microbiology & Immunology. Elsevier Health Sciences. pp. 88–89. ISBN 978-8131236246. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ Detels R, Gulliford M, Karim QA, Tan CC (2015). Oxford Textbook of Global Public Health. Oxford University Press. p. 1490. ISBN 978-0199661756. Archived from the original on 1 May 2021. Retrieved 30 March 2015.
- ^ Demicheli V, Barale A, Rivetti A (July 2015). "Vaccines for women for preventing neonatal tetanus". The Cochrane Database of Systematic Reviews. 2015 (7): CD002959. doi:10.1002/14651858.CD002959.pub4. PMC 7138051. PMID 26144877.
- ^ Swamy GK, Garcia-Putnam R (February 2013). "Vaccine-preventable diseases in pregnancy". American Journal of Perinatology. 30 (2): 89–97. doi:10.1055/s-0032-1331032. PMID 23271378. S2CID 206342684.
- ^ Bärnighausen T, Bloom DE, Cafiero-Fonseca ET, O'Brien JC (August 2014). "Valuing vaccination". Proceedings of the National Academy of Sciences of the United States of America. 111 (34): 12313–9. Bibcode:2014PNAS..11112313B. doi:10.1073/pnas.1400475111. PMC 4151736. PMID 25136129.
- ^ a b c Deogaonkar R, Hutubessy R, van der Putten I, Evers S, Jit M (October 2012). "Systematic review of studies evaluating the broader economic impact of vaccination in low and middle income countries". BMC Public Health. 12: 878. doi:10.1186/1471-2458-12-878. PMC 3532196. PMID 23072714.
- ^ a b Jit M, Newall AT, Beutels P (April 2013). "Key issues for estimating the impact and cost-effectiveness of seasonal influenza vaccination strategies". Human Vaccines & Immunotherapeutics. 9 (4): 834–40. doi:10.4161/hv.23637. PMC 3903903. PMID 23357859.
- ^ a b c * Hinman AR, Orenstein WA, Papania MJ (May 2004). "Evolution of measles elimination strategies in the United States". The Journal of Infectious Diseases. 189 (Suppl 1): S17-22. doi:10.1086/377694. PMID 15106084.
*Sencer DJ, Dull HB, Langmuir AD (March 1967). "Epidemiologic basis for eradication of measles in 1967". Public Health Reports. 82 (3): 253–6. doi:10.2307/4592985. JSTOR 4592985. PMC 1919891. PMID 4960501. - ^ van Boven M, Kretzschmar M, Wallinga J, O'Neill PD, Wichmann O, Hahné S (November 2010). "Estimation of measles vaccine efficacy and critical vaccination coverage in a highly vaccinated population". Journal of the Royal Society, Interface. 7 (52): 1537–44. doi:10.1098/rsif.2010.0086. PMC 2988255. PMID 20392713.
- ^ Robertson, David (10 June 2021). "Of Mice and Schoolchildren: A Conceptual History of Herd Immunity". American Journal of Public Health. 111 (8): e1–e8. doi:10.2105/AJPH.2021.306264. PMC 8489650. PMID 34111938. S2CID 235404539.
- ^ Hedrich AW (1933). "Monthly Estimates of the Child Population Susceptible to Measles, 1900–1931, Baltimore, Md". American Journal of Epidemiology. 17 (3): 613–636. doi:10.1093/oxfordjournals.aje.a117929.
- ^ Strassburg MA (May 1982). "The global eradication of smallpox". American Journal of Infection Control. 10 (2): 53–9. doi:10.1016/0196-6553(82)90003-7. PMID 7044193.
External links[edit]
- Topley WW, Wilson GS (May 1923). "The Spread of Bacterial Infection. The Problem of Herd-Immunity". The Journal of Hygiene. 21 (3): 243–9. doi:10.1017/s0022172400031478. PMC 2167341. PMID 20474777.
- A visual simulation of herd immunity written by Shane Killian and modified by Robert Webb
- Herd immunity simulation






